Platelet Rich Plasma Injection
Platelet rich plasma injections involve injecting a patient’s own platelets concentrated from blood into areas of injury or degeneration to potentially stimulate healing. PRP contains growth factors and cytokines that modulate inflammation and promote tissue regeneration
How Does Platelet Rich Plasma Injection Work?
Treatment consists of the patient getting a Platelet Rich Plasma injection directly into the joint or tendon. This minimal invasive outpatient treatment takes about one hour to perform. It’s generally performed 1-3 times for maximum effectiveness. Blood is mostly made up of liquid known as plasma. Yet, it also has tiny, solid particles such as white cells, red cells and platelets. Your platelets play a very important part in clotting your blood. They also contain hundreds of proteins referred to as growth factors. These proteins are instrumental in healing injuries.
How is Platelet Rich Plasma Prepared?
Here’s how the Platelet Rich Plasma is Prepared:
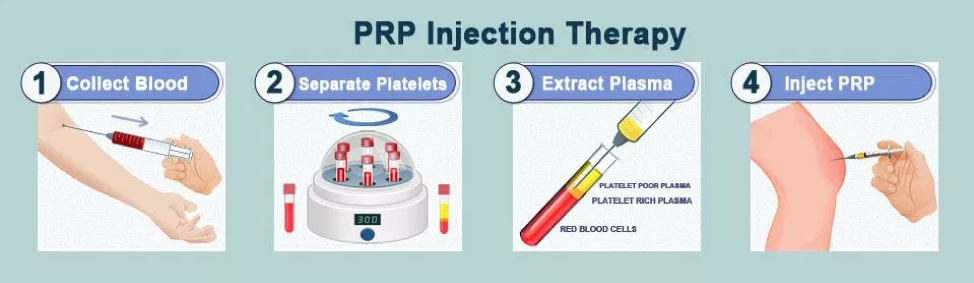
- Patient’s blood is drawn.
- Platelets are separated from the white and red blood cells.
- Concentration of the platelets is increased during the “centrifugation” process.
- Increased platelets concentration combined with the body’s remaining blood through PRP injection.
How Does a Platelet Rich Plasma Injection Take Place?
In order for a Platelet Rich Plasma injection to be effective, the injury site must be treated in one of two fashions:
- Patient can receive a Platelet Rich Plasma injection directly to the injured area. A local anesthetic can be used in combination with the PRP injection to ease pain or discomfort.
- A Platelet Rich Plasma injection can be used to help with healing after surgery due to injury. A torn heal is a prime example. After such an injury, surgery may be necessary to repair the tendon. Treating the injured area with a Platelet Rich Plasma injection during surgery can improve healing.
What Conditions is PRP Effective at Treating?
A number of peer-reviewed studies have shown that PRP is often powerfully effective with healing various injuries. Just how effective it is depends on the area being treated and the patient’s overall health. Whether the injury was caused by an accident or trauma (acute) or has developed over time (chronic) also plays a factor in the effectiveness of Platelet Rich Plasma injections. Some of the conditions that have shown great improvement after being treated using Platelet Rich Plasma injection include:
- Surgery
- Fractures
- Knee Arthritis
- Acute Ligament and Muscle Injuries
- Chronic Tendon Injuries
Platelet Rich Plasma injections have been known to beat out the competitive techniques, such as hyaluronic acid in several tests. Other remedies that have shown promise with healing injuries and after surgery include bone marrow stem cell injections and, of course, traditional orthopedic surgery. For more information on Platelet Rich Plasma injection, contact us here at the San Diego Orthopedic Surgery Clinic today.
Indications and Patient Selection
PRP injections may be considered for various orthopedic conditions including knee osteoarthritis, tendinopathies, acute muscle injuries, and ligament or tendon tears[2]. Patients are typically those who have failed other conservative treatments. Contraindications include platelets disorders, some malignancies, active infections, and use of anticoagulants[3].
PRP Preparation
PRP preparation involves collecting a patient’s venous blood and centrifuging it to isolate and concentrate the platelets from the red blood cells and plasma[4]. This can be done at bedside using specialized PRP centrifugation systems that yield 3-8x higher platelet concentrations than whole blood. Anticoagulants like citrate are added to prevent clotting. The final PRP volume is typically 2-6mL.
PRP Injection Procedure
The area to be injected is identified and prepared sterilely. Local anesthetics may be injected prior for pain control. Under ultrasound or fluoroscopic guidance, the PRP injection is slowly administered using a 22-25 gauge needle[5]. Common injection sites are the knee joint, tendons, ligaments, or areas of muscle injury. Pressure is applied after to prevent bleeding.
PRP Post-Injection Care
Patients are monitored for 30-60 minutes after injection. Mild swelling, bruising, stiffness, and pain are common initially[6]. NSAIDs, ice, elevation, and rest help manage symptoms. Gradually resuming activity based on a structured rehabilitation program is recommended. Therapeutic effects may take several weeks to months to maximize. Repeat injections may be considered if initial response is inadequate.
Evidence for Use
Moderate evidence supports PRP for knee osteoarthritis and tendinopathies like tennis elbow, plantar fasciitis, and Achilles tendinitis[7]. Evidence is weaker for muscle strains and ligament injuries. Outcomes are best for mild pathology versus late stage disease. Combining PRP with physiotherapy may have added benefits. More research is still needed to optimize PRP protocols.
Benefits and Risks
Benefits include potential for symptomatic relief and tissue healing without surgery. It is minimally invasive and uses the patient’s own blood. Risks are low but include pain, infection, and no improvement[8]. Rare risks are bleeding, tissue damage from injection, and post-injection flare. Costs are out-of-pocket since insurance coverage is limited.
In summary, meticulous sterile technique and proper patient selection help maximize outcomes from PRP injections. While promising, more research is still needed to determine their ideal role in orthopedic treatment.
The role of PRP in knee osteoarthritis:
Knee Osteoarthritis
Osteoarthritis (OA) is a degenerative joint disease characterized by the breakdown of articular cartilage, joint space narrowing, osteophyte formation, and subchondral sclerosis. It is the most common form of arthritis and a leading cause of disability worldwide.
Knee OA is particularly prevalent, affecting approximately 10% of men and 13% of women over the age of 60[2]. Symptoms include pain, stiffness, swelling, and decreased range of motion. Risk factors include obesity, previous joint injury, genetics, and aging[3]. Knee OA can significantly impact quality of life if not managed appropriately.
Overview of PRP
Platelet-rich plasma (PRP) is an autologous concentration of platelets in a small volume of plasma. Platelets contain growth factors and other proteins that regulate healing and regeneration. PRP is prepared from a patient’s own blood and then injected back into the damaged site to potentially augment healing[4].
It is theorized that the growth factors released from the concentrated platelets may reduce inflammation, increase collagen production, recruit stem cells, and stimulate regeneration in areas of injury or degeneration[5]. PRP has been extensively studied as a potential treatment approach for musculoskeletal conditions, including knee OA.
Efficacy of PRP for Knee Osteoarthritis
Several randomized controlled trials have evaluated the efficacy of PRP injections for knee OA. In one study, patients received either a single PRP injection or placebo[6]. At 6 months, the PRP group showed significantly better outcomes in terms of pain, symptoms, and quality of life.
A recent meta-analysis pooled data from 14 randomized trials, with a total of 1,077 patients[7]. PRP resulted in significantly greater improvements in pain and physical function compared to hyaluronic acid and placebo control injections. The benefits were still present at 12 months.
However, some studies show no benefit of PRP over other injections. A trial of 218 patients found no differences between PRP and hyaluronic acid injections at 6 and 12 months[8]. Several factors could impact efficacy, including PRP preparation methods, frequency of injection, and severity of OA. More research is still needed to compare PRP to established therapies and determine optimal protocols.
Overall, there is moderate evidence that PRP provides mild to moderate benefits for knee OA symptoms. It is considered a safe, low risk intervention. PRP likely works best for mild to moderate OA and when combined with physical therapy or lifestyle modifications. More studies are needed to fully determine its appropriate clinical role.
PRP injection for Elbow Lateral Epicondylitis
Introduction
Lateral epicondylitis, also known as tennis elbow, is a common cause of elbow pain caused by overuse. It involves microtearing of the extensor carpi radialis brevis tendon at the lateral epicondyle.1 Understanding this condition is key for proper treatment.
Pathophysiology
Repetitive wrist extension and forearm supination during activities like tennis, golf, and occupational overuse also risk lateral epicondylitis. This leads to microscopic tears at the origin of the extensor carpi radialis brevis tendon.2 Inflammation follows, with release of cytokines and pain mediators. Microruptures exceed the tendon’s healing capacity.
Clinical Presentation
Patients report lateral elbow pain that is aggravated by grasping or lifting activities and often awakens them from sleep.3 On exam, palpation elicits epicondyle tenderness. Resisted wrist extension and passive wrist flexion reproduce symptoms. Advanced cases demonstrate tendon thickening and granulation.
Imaging
Radiographs rule out bony abnormalities but do not show soft tissue changes of lateral epicondylitis. MRI or ultrasound can identify tendinosis, tears, calcifications, and synovial hypertrophy.4 However, findings frequently exist in asymptomatic patients as well, complicating diagnosis.
Conservative Treatment
Activity modification, counterforce bracing, physical therapy focused on eccentric strengthening, massage, and anti-inflammatories provide initial pain relief and healing promotion for most patients over 6-12 months.5 Corticosteroid injections offer short-term benefit but delay overall recovery.
Refractory Cases
For cases failing conservative treatment, options include shockwave therapy, platelet-rich plasma injections to stimulate healing, and a tenex procedure to debride degenerated tissue. Open or arthroscopic repair is reserved for complete tendon tears.6
In summary, lateral epicondylitis causes significant functional impairment of the dominant arm. A majority of patients improve with rest, therapy, and activity modifications. Those who remain symptomatic may benefit from advanced treatments like PRP or surgery.
Role of PRP in Orthopedics and Sports Medicine
Introduction
Platelet-rich plasma (PRP) aims to promote healing through high concentrations of autologous growth factors. Potential applications in orthopedics and sports medicine include treating tendinopathy, muscle injuries, ligament sprains, arthritis, and augmenting surgical repairs.1 Multiple studies analyze the efficacy and appropriate uses of PRP.
Tendinopathy
For chronic tendinopathies like tennis elbow, rotator cuff, Achilles, and patellar tendinitis, PRP injections consistently demonstrate improved pain and function scores versus controls over 1-3 year follow-up.2 However, evidence of collagen repair on imaging is lacking. PRP may modulate inflammation rather than fundamentally alter degeneration.
Muscle Injuries
Moderate muscle strains of the hamstrings, quadriceps, and calf show faster return to play and reduced risk of reinjury after PRP injection versus controls.3 Pain during rehabilitation is also decreased. The anti-inflammatory effects likely facilitate earlier mobilization and recovery.
Ligament Sprains
In acute ankle sprains, PRP injections do not reduce short-term swelling and pain compared to placebo.4 However, RF studies show improved mechanical properties of the ankle ligaments with PRP, suggesting possible injury reduction. Effects on knee MCL and LCL sprains require further study.
Osteoarthritis
Intraarticular PRP injections provide significant but transient (6-12 months) pain relief in knee osteoarthritis and chondral defects based on high-quality trials.5 Impact on disease progression is lacking. Repeated PRP injections can maintain symptom relief.
Surgical Augmentation
Small RCTs show promise for PRP in augmenting rotator cuff and ACL reconstruction to improve tendon-bone healing.6 PRP application during microfracture, meniscal repair, and chondral scaffold implantation may also improve outcomes, though robust data is lacking. Further research on formulation, timing, and delivery of PRP for augmentation is needed.
In summary, moderate evidence supports integrating PRP injections into multimodal treatment for tendinopathy and muscle strains. More research is required to clarify the optimal role in ligament injuries, arthritis, and surgical applications. Regulatory standards for PRP preparation may help advance the field.
Role of PRP in Shoulder Bursitis
Introduction
Shoulder bursitis involves inflammation of the subacromial-subdeltoid bursa that overlies the rotator cuff and humeral head. This can cause shoulder pain, limited mobility, and difficulty with overhead activities.1 Injectable treatments like corticosteroids and platelet-rich plasma (PRP) aim to reduce inflammation and enhance healing.
Pathogenesis
Repetitive shoulder overuse or injury causes inflammation and swelling of the subacromial bursa. This impinges and irritates the rotator cuff tendons. Fluid accumulation within the bursa limits mobility and contributes to subacromial impingement. Inflamed bursal tissue also releases pro-inflammatory cytokines that sensitize local pain receptors.
Rationale for PRP
Growth factors concentrated in PRP could help resolve bursal inflammation and promote healing by stimulating bursal fibroblasts and modulating immune cells.2 PRP also improves rotator cuff tendon integrity based on animal studies. These mechanisms provide a rationale for studying PRP in shoulder bursitis.
Efficacy of PRP Injections
Multiple randomized trials show PRP injections significantly improve shoulder pain and function in subacromial bursitis without adverse effects.3 Improvements persist over 6-12 months compared to placebo or steroid injections. PRP also appears superior to exercise therapy alone. Repeated PRP injections can extend benefits.
Limitations of Evidence
Optimal PRP formulations and injection regimens need further study. Whether PRP offers long-term modification versus just symptom relief is also unclear. High-quality multi-center trials with imaging outcomes could strengthen the evidence for PRP in shoulder bursitis.
In summary, current evidence supports PRP as an effective treatment option for shoulder bursitis refractory to conservative treatment. PRP injections can provide sustained reductions in pain and improvements in mobility compared to other injectables. Further research could help optimize PRP therapy protocols.









