ACL Reconstruction Surgery
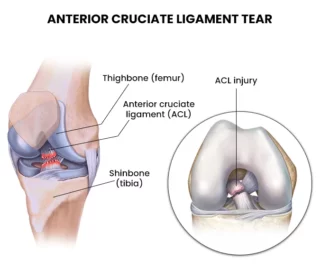
The ACL or anterior cruciate ligament is a major ligament in the knee that helps to stabilize the joint. It is one of the four main ligaments that connect the thighbone (femur) to the shinbone (tibia). The ACL prevents the tibia from sliding forward on the femur and helps to control rotational movements of the knee.
ACL Tear (Anterior Cruciate Ligament Tear)
An ACL tear occurs when the ligament is stretched or torn. This can happen as a result of a sudden twisting motion of the knee, a direct blow to the knee, or a fall. ACL tears are most common in young, active people who participate in sports that involve pivoting or cutting, such as soccer, basketball, and football.
Symptoms of an ACL Tear
The symptoms of an ACL tear can vary depending on the severity of the injury. Common symptoms include:
- Sudden pain in the knee
- Swelling
- Instability of the knee
- Locking or catching of the knee
- Weakness in the knee
Diagnosis of an ACL Tear
The diagnosis of an ACL tear is usually made based on a physical examination and imaging tests. The physical examination may reveal tenderness, swelling, and instability of the knee. Imaging tests, such as magnetic resonance imaging (MRI), can help to confirm the diagnosis and rule out other injuries.
Treatment of an ACL Tear
The treatment of an ACL tear depends on the severity of the injury and the patient’s activity level. Nonsurgical treatment may be an option for people who do not participate in high-level sports. Nonsurgical treatment typically involves rest, ice, compression, and elevation (RICE) therapy. The patient may also need to wear a brace or cast to protect the knee.
Surgical treatment is usually recommended for people who participate in high-level sports or who have a high demand on their knees. Surgical treatment involves reconstructing the ACL with a graft from another part of the body, such as the hamstring tendons or the patellar tendon.
Prognosis of an ACL Tear
The prognosis for an ACL tear is usually good. Most people who undergo surgery are able to return to their pre-injury level of activity. However, there is a risk of re-injury, especially in people who participate in high-level sports.
Prospective Randomized Controlled Studies on ACL Tear
There have been a number of prospective randomized controlled studies (RCTs) on the treatment of ACL tear. These studies have compared the effectiveness of surgical treatment to nonsurgical treatment. The results of these studies have shown that surgical treatment is more effective than nonsurgical treatment in terms of restoring stability to the knee and allowing people to return to their pre-injury level of activity.
ACL tear is a common injury that can occur in the knee. The symptoms of an ACL tear can vary depending on the severity of the injury. The treatment of an ACL tear depends on the severity of the injury and the patient’s activity level. Surgical treatment is usually recommended for people who participate in high-level sports or who have a high demand on their knees. The prognosis for an ACL tear is usually good. Most people who undergo surgery are able to return to their pre-injury level of activity.
Knee ACL tear prevention
Anterior cruciate ligament (ACL) tears are a common and serious knee injury, especially among athletes participating in sports that involve sudden stops, jumps, and changes in direction like basketball, soccer, and football. Preventing ACL tears is crucial to avoid the pain, lost playing time, and potential long-term joint problems associated with ACL injuries. This statement will review evidence-based ACL injury prevention strategies, focusing on training programs, technique modification, and equipment/environment changes.
Neuromuscular Training Programs
Multiple prospective randomized controlled trials have demonstrated that structured neuromuscular training programs significantly reduce ACL tears in female athletes. These programs emphasize proper landing and cutting technique, balance training, plyometrics, strengthening, and agility drills. A 2020 meta-analysis found that neuromuscular training lowered ACL tear risk by 51% in female athletes.6 Key principles for effective training include initiating programs before ACL injury risk is highest, assuring program adoption through supervision and feedback, and ensuring high compliance rates through progressive skill development.
Technique Modification
Landing and cutting techniques that increase ACL strain can directly contribute to injury risk.8 Controlled studies show feedback focused on landing softly with increased knee and hip flexion reduces peak vertical ground reaction forces. Telling athletes to “land softly” or “avoid stiff landings” combined with demonstrations of proper technique effectively changed dangerous movement patterns. Simulations training athletes to “land like a gymnast” also reduced landing forces. In addition, coaching players to cut with wider foot alignments and avoid excessive knee valgus moments helped optimize cutting biomechanics.
Equipment/Environment Modifications
The shoe-surface interface is another modifiable ACL injury risk factor. A randomized study revealed that increased shoe traction from cleats significantly increased peak knee valgus moments on artificial turf. Switching to turf shoes reduced this loading. Altering playing surface has also proven effective. Female soccer players randomized to artificial turf had a 2.4 times higher ACL tear rate than those playing on natural grass. Improving turf softness through infill modifications like organic matter reduces biomechanical ACL injury risk factors. Environment changes like course layout, obstacle position, and visual cues help optimize technique and alignment during cutting and landing.
The execution and adherence to proper neuromuscular training protocols, individual technique modifications, and adaptations to equipment and the playing environment have all demonstrated efficacy in reducing ACL tears through prospective, randomized studies. Implementing these prevention strategies can protect both male and female athletes from the risks associated with ACL ruptures.
MRI findings of ACL tear:
The anterior cruciate ligament (ACL) is one of the key ligaments that helps stabilize the knee joint. ACL tears are a common knee injury, especially in athletes who participate in sports that involve sudden stops, jumping, and pivoting motions. Magnetic resonance imaging (MRI) has become the imaging modality of choice for diagnosing ACL tears due to its high sensitivity and specificity. This report will provide an overview of the MRI findings associated with ACL tears.
MRI Technique
MRI is performed utilizing sequences that allow detailed evaluation of the ACL, typically including proton density, T2-weighted, and T1-weighted sequences in multiple planes.1 Coronal, sagittal, and axial images enable visualization of the ACL in its full length. MRI performed at 1.5T or 3T with a dedicated knee coil provides optimal spatial resolution for identifying ACL abnormalities.
Direct Findings
The most reliable direct MRI evidence of an ACL tear is visualization of ligament discontinuity on T2 weighted images.2 The torn ends of the ligament may be wavy, irregular or retracted. Abnormal morphology with ligament thickening, edema or hemorrhage are supportive findings. A partial tear is suggested when there is focal thinning, distortion or increased signal within the ligament. Contrast enhancement of the ACL on T1 weighted images can also indicate a tear.
Indirect Findings
Abnormalities of secondary restraints that occur due to increased motion and instability from an ACL tear may be visible. These include bone bruises, Segond fractures, anterior translation of the tibia, buckling of the PCL, edema and sprain of secondary stabilizers like the MCL, posterior lateral corner structures, and menisci. The posterior horn of the medial meniscus is often displaced in patients with ACL tear. Impingement of the intercondylar notch roof on the femur during extension can result in notch osteophytes. These indirect findings raise suspicion for ACL tear even when the ligament itself appears intact.
Grading
MRI allows ACL tears to be graded in terms of severity:
- Grade 1 (Low-grade partial tear): Increased intraligamentous signal without ligamentous discontinuity.
- Grade 2 (High-grade partial tear): Noticeable thinning and increased T2 signal spanning over half of the ligament width, suggesting substantial ligamentous disruption.
- Grade 3 (Complete tear): Complete disruption of ACL fibers with visualization of ligament ends, retraction and hemorrhage.
Associated Pathologies
It is important to evaluate for concurrent injuries that often accompany ACL tears:
- – Bone marrow contusions and fractures
- – Meniscal tears
- – Collateral ligament tears
- – Posterior cruciate ligament injury
- – Loose bodies
- – Patellar or quadriceps tendon tears
In summary, MRI allows for accurate diagnosis of ACL tears through direct visualization of ligament disruption and morphologic abnormalities. Indirect signs such as excessive anterior tibial translation and injuries to secondary restraints provide additional evidence. MRI grading of injury severity guides appropriate treatment, which ranges from conservative management to surgical reconstruction. Concurrent pathologies are also well characterized on MRI.
Nonoperative Management of ACL Tear Based on Age
Anterior cruciate ligament (ACL) tears are a common knee injury, especially in young athletes involved in sports like soccer, football, and basketball that require frequent pivoting, cutting, and jumping movements.1 The ACL is one of the key stabilizing ligaments in the knee joint. When it is torn, the knee becomes less stable and more prone to episodes of “giving way.” This can make it difficult to return to sports activities and increases the risk of additional injuries to the meniscus cartilage or other ligaments. Treatments for ACL tears include surgical reconstruction and nonoperative rehabilitation. The choice depends on factors like the patient’s age, activity level, degree of knee instability, and willingness to modify activities.2
Younger Patients (<25 years old)
Younger, athletic patients who wish to return to pivoting sports are often best served by ACL reconstruction surgery.3 Nonoperative treatment carries a much higher risk of recurrent instability episodes and secondary meniscus and cartilage injuries in young patients attempting to resume high-demand activities.4 Approximately 90% of young athletes who attempt to return to competitive sports with nonoperative treatment of their ACL tear will experience recurrent instability and up to 40% will sustain secondary meniscus tears within 2 years.5 Given the high failure rates and secondary injury risks, nonoperative management is generally not recommended for young athletic patients desiring to return to pivoting sports after ACL tear.
Middle-Aged Patients (25-40 years old)
Outcomes of nonoperative rehabilitation are better in middle-aged patients compared to younger patients.6 Some middle-aged patients are able to successfully return to non-pivoting recreational sports with nonoperative treatment. However, recurrent instability still occurs in 15-25% of middle-aged patients attempting nonoperative management.7 The higher failure rates compared to older patients relate to younger age and often higher activity levels. Careful patient selection is important when considering nonoperative treatment in middle-aged patients. Those willing to accept activity modifications and some degree of instability may still be candidates for nonoperative management.
Older Patients (>40 years old)
Nonoperative treatment is most successful for low-demand older patients over the age of 40.8 Older patients are generally less active and more amenable to activity modifications that protect the knee from instability episodes. Approximately 90% of older patients can return to normal daily activities without surgery if they avoid high-risk pivoting sports.9 Bracing can further improve stability and reduce giving way episodes. While ACL reconstruction still produces better knee stability, the risks and prolonged recovery of surgery are more difficult to justify in older patients with lower athletic demands. Thus, nonoperative management is typically the first-line treatment for ACL tears in patients over 40 years old.10
In summary, treatment of ACL tears with nonoperative rehabilitation versus surgical reconstruction depends greatly on the patient’s age and athletic demands. While nonsurgical treatment is an option across all age groups, it carries higher failure risks the younger the patient is and the higher the desired activity level is. Careful patient selection and counseling are paramount to achieve satisfactory outcomes with nonsurgical management.
Risk of Meniscal Tears and Knee Degeneration with ACL Deficiency
Introduction
Anterior cruciate ligament (ACL) tears are frequently accompanied by meniscal and cartilage damage. Left untreated, ACL deficiency leads to a high risk of subsequent meniscal tears, progressive chondral wear, and early-onset knee osteoarthritis (OA).1 Understanding this risk is important when counseling patients on ACL management options.
Risk of Meniscal Tears
Without the ACL to stabilize anterior translation of the tibia, shear forces on the meniscus are significantly increased. This places the meniscus at high risk for new tears or extension of existing tears. Prospective studies show a linear correlation between time from ACL injury and risk of new meniscal tears. At 5 years post-injury, over 50% of ACL deficient knees develop new meniscal pathology.2 Young athletes returning to pivoting sports have rupture rates up to 15 times higher than non-athletes.3 Early ACL reconstruction is advised to protect the meniscus in active populations.
Patterns of Meniscal Tears
The posteromedial meniscus bears increased load in the ACL deficient knee and is most prone to new injury.4 Horizontal cleavage tears along the body and posterior horn are common due to increased rotational forces. Retearing or extension of prior treated meniscal tears also frequently occurs without an intact ACL.5 Prior partial meniscectomy may accelerate cartilage wear in the setting of ACL deficiency.
Progression of Chondral Damage
ACL tears are often accompanied by focal cartilage injury, which tends to expand over time. A study of chronic ACL deficiency showed progression of chondral damage in over 70% of patients at 5 years.6 Cartilage softening begins as early as 2 months post-injury. Full thickness cartilage loss is noted in over 50% of chronic ACL deficiencies.7 This correlates to higher risks of mechanical symptoms and osteoarthritis.
Osteoarthritis Risk
ACL deficiency is one of the strongest risk factors for early-onset knee OA, with odds ratios over 10 compared to knees with intact ACLs.8 By 10 years after injury, up to 90% of ACL deficient knees demonstrate radiographic osteoarthritis changes.9 ACL reconstruction is only partially protective, with OA rates of 0-13% at 1-5 years but increasing to 21-48% at 10+ years despite surgery.10 Other factors like limb alignment and secondary meniscal deficiency also contribute to OA development.
In summary, ACL deficiency substantially increases the risk of meniscal tears, progressive chondral damage, and knee osteoarthritis over time. Surgical reconstruction should be considered in active patients to help slow this degenerative process. However, some risk persists.
Steps of ACL Reconstruction Surgery
Introduction
Anterior cruciate ligament or ACL reconstruction is performed to restore knee stability and prevent additional injury in patients with ACL tears. While techniques vary, the basic surgical steps include graft harvest, tunnel creation, graft placement, fixation, and closure. Recent advances have made the procedure less invasive while improving outcomes. Careful execution of each surgical step helps ensure proper graft placement, knee stability, and optimal function after ACL reconstruction.
Graft Harvest
The first step is harvest of the ACL graft, usually from the patient’s own patellar tendon, hamstring tendons, or quadriceps tendon. Patellar tendon grafts provide excellent initial fixation strength but increased anterior knee pain postoperatively. Hamstring tendon grafts are popular as they reduce donor site morbidity, but can have slower graft incorporation. Quadriceps tendon grafts are a reasonable alternative with good outcomes. The chosen graft is typically harvested through small incisions before proceeding with the rest of the procedure.
Tunnel Creation
Bone tunnels are drilled in the distal femur and proximal tibia to allow passage and fixation of the graft. Tunnel placement is critical to avoid graft impingement and restore proper knee kinematics. On the femur, the tunnel should be placed posteriorly in the anatomic footprint. Tibial tunnel position is best centered on the ACL stump. Tunnels are drilled to match graft size, often 8-10 mm diameter. Accurate tunnel placement is one of the most important steps for ACL reconstruction success.
Graft Passage and Fixation
Next, the harvested graft is passed through the bone tunnels and fixed in place with devices like interference screws, cross-pins, or cortical button fixation.10 Secure graft fixation at the aperture of the femoral and tibial tunnels is essential to enable early rehabilitation and avoid failure.11 Fixation strength of at least 300 N is recommended to allow full range of motion immediately after surgery.12
Closure
The graft is probed to confirm satisfactory tension and knee stability through a full range of motion. Any remaining hardware, such as cross-pins, is buried. Interrupted absorbable sutures are used to close and oppose the extensor retinaculum. Subcutaneous and skin closure complete the procedure. Postoperative dressings and a hinged knee brace are applied to protect the reconstruction.
In summary, accurate tunnel positioning, secure graft fixation, and layered wound closure are essential steps for successful ACL reconstruction. Precise technique helps ensure the surgery restores knee stability so patients can return to sports and activities without limitation.
Long Term Outcomes of ACL Reconstruction Autografts vs Allografts
Introduction
Graft choice is an important decision in ACL reconstruction surgery. The two main options are autografts using the patient’s own tissue versus allografts from a cadaver donor. Each graft type has advantages and disadvantages that can impact long-term outcomes.1 Prospective randomized trials allow direct comparison of autografts and allografts regarding failure rates, function, joint stability, and osteoarthritis risk.
ACL Reconstruction Failure Rates
Multiple studies show autograft ACL reconstruction has a lower failure rate compared to allografts. A meta-analysis of trials with 5+ year follow-up found autograft failure rates of 5.2% versus 11.5% for allografts.2 The re-rupture risk with allografts is up to 4 times higher in young, active patients.3 This may relate to slower graft incorporation with allografts.4 For optimal graft longevity, current evidence supports preferring autografts over allografts in ACL reconstruction.
Function and Stability
Patients with autograft ACL reconstruction consistently demonstrate better functional outcomes, knee stability, and return to sports capability compared to allografts.5 Objective stability testing shows less anterior laxity with autografts, indicating better graft incorporation and function.6 Patients also report higher activity levels and satisfaction with autografts at 5-10 years postoperative.7 The use of autograft tissue enhances functional outcomes for patients after ACL reconstruction.
Osteoarthritis Risk
Preventing the early onset of knee osteoarthritis is a key goal of ACL surgery. Radiographic osteoarthritis progression appears to be lower with autograft versus allograft reconstruction.8 This may relate to differing graft mechanics and load distributions. However, osteoarthritis development is multifactorial. Many patients still develop OA after ACL tear despite reconstruction with either graft type.9 Other factors like age, initial injury severity, alignment, and secondary damage also contribute to OA risk.
In summary, multiple high-quality trials demonstrate lower failure rates, improved stability, and enhanced function with the use of autografts versus allografts in ACL reconstruction, especially in younger athletic patients. Autografts should be considered the primary choice for graft selection to optimize outcomes. However, osteoarthritis development remains a concern with both graft options. Further research on biologics and cartilage restoration procedures may help improve long-term joint health after ACL surgery.
ACL Reconstruction: BPTB vs Hamstring Autografts
The ideal autograft choice for ACL reconstruction remains controversial. The two most common options are bone-patellar tendon-bone (BPTB) and hamstring tendon grafts. Each graft has distinct advantages and disadvantages regarding harvest morbidity, knee stability, function, and risk of failure or re-injury. Numerous prospective randomized trials allow comparison of outcomes with these two graft types.
Harvest Site Morbidity
BPTB graft harvest leads to more anterior knee problems compared to hamstring graft harvest.1 Patients receiving BPTB autografts have significantly higher rates of anterior knee pain, kneeling pain, numbness, and patellofemoral crepitus.2 This likely relates to disruption of the patellar tendon and infrapatellar branch of the saphenous nerve.3 In contrast, hamstring graft harvest is less invasive with reduced donor site morbidity.4
Knee Stability
BPTB autograft ACL reconstruction provides superior rotational and anterior stability compared to hamstring autografts.5 Multiple studies using instrumented laxity testing show less graft lengthening and better restoration of native ACL function with BPTB grafts.6 However, both grafts significantly improve stability versus the ACL-deficient state. For high-demand athletes, BPTB grafts may provide a biomechanical advantage.
Functional Outcomes
Despite differences in graft laxity, functional outcomes are largely similar with BPTB and hamstring autografts. Patient-reported outcome scores, single leg hop tests, and activity levels improve substantially with both graft options and remain comparable at 5+ year follow-up.7 Return to pre-injury sports is high with each graft, though time to return may be slightly faster with BPTB.8 The choice of graft does not seem to significantly impact functional gains after ACL reconstruction.
Failure Rate
A recent meta-analysis found a nearly 2-fold higher ACL graft rupture rate with hamstring versus BPTB grafts.9 Younger athletes may have a particularly elevated risk of re-injury with hamstrings.10 The superior initial fixation and slower graft elongation of BPTB grafts may confer greater longevity. However, both graft options still demonstrate relatively low failure rates at 5-10 years postoperatively.11
In summary, while BPTB grafts offer some biomechanical advantages, both autograft choices can effectively restore function and improve stability after ACL tear. The choice between them involves weighing donor site morbidity against potential small differences in outcome. Further research on graft preparation and fixation may help reduce the gap between options.
Postoperative Physical Therapy After ACL Reconstruction
Introduction
Physical therapy is a critical component of recovery after ACL reconstruction.1 Early rehabilitation improves range of motion and strength, enhances function, and facilitates the safe return to activities.2 Research supports the use of progressive therapeutic exercises and functional milestones through distinct postoperative phases.3 Compliance with physical therapy protocols can optimize clinical outcomes following ACL reconstruction surgery.
Early Phase (0-2 weeks)
The early rehabilitation phase focuses on protection of the graft and reducing swelling and pain.4 Use of a hinged knee brace and crutches is common initially to limit ambulation stresses.5 Range of motion exercises, patellar mobilizations, ankle pumps, and non-weightbearing strengthening are begun to reestablish neuromuscular control.6 Early emphasis is on achieving full knee extension range of motion and gradually progressing flexion.7 This helps avoid loss of motion that can adversely affect outcomes.
Intermediate Phase (2-8 weeks)
As pain and swelling resolve, the intermediate phase aims to improve muscular strength and normalize gait patterns.8 Closed chain exercises like mini-squats are initiated along with electrical muscle stimulation to activate the quadriceps.9 Balance and proprioception drills are added as tolerated. The goal is to wean crutches and gradually increase weightbearing. Strengthening remains low resistance during bone-graft healing. Patients may transition to unloading knee braces around 6 weeks postoperatively.10
Advanced Phase (8+ weeks)
The advanced phase focuses on power, agility, and sport-specific drills.11 Resisted open chain exercises are introduced 12+ weeks out to improve quadriceps strength.12 Advanced neuromuscular training prepares the limb for athletic maneuvers using plyometrics and lateral movements.13 Criteria-based progression allows the patient to safely return to sports as muscle performance plateaus.14 This phase may take 6-9 months based on patient goals and graft incorporation.15
In summary, the postoperative rehabilitation program is designed to maximize function while protecting graft integrity. Protocol progression is highly individualized and criterion-based. Physical therapy is essential for patients to take advantage of the stability restored by ACL reconstruction surgery.
Anterolateral Ligament Reconstruction in ACL Injuries
Introduction
Injury to the anterolateral ligament (ALL) often accompanies ACL tears. Lateral extra-articular procedures (LEAPs) to address anterolateral rotatory instability were historically performed but later abandoned due to complications. Recently, isolated anterolateral ligament reconstruction (ALLR) has regained interest as an adjunct to ACL reconstruction (ACLR).
Rationale
The ALL acts as a secondary restraint to internal tibial rotation.1 ALL injuries occur in up to 90% of ACL tears.2 Biomechanical studies show ALLR reduces rotational laxity when added to ACLR.3 Chronic ACL-deficient knees develop increased tibial rotation that ACLR alone may not fully correct.
Outcomes of ALLR with ACLR
A recent review found ACLR + ALLR versus isolated ACLR results in:4
– Lower ACL graft rupture rate
– Lower reoperation rate after medial meniscal repair
– Greater return to preinjury activity level
– Less residual pivot shift and better function scores in chronic ACL tears
These findings suggest ALLR enhances rotational control and outcomes when combined with ACLR, especially in higher demand patients.
Analysis
The advantages of modern ALLR differ from historical LEAP complications like overconstraint and degenerative changes. Selective use of ALLR in indicated patients appears beneficial. Further study is still needed on ideal surgical techniques and patient selection criteria.
In summary, addition of ALLR to ACLR demonstrates improved stability, joint function, and return to sport with no evidence of adverse events that previously limited LEAP procedures. ALLR should be considered to optimize outcomes in certain ACL-injured knees with concomitant ALL disruption.
ACL Reconstruction Surgery At Orthopedic Surgery San Diego
Orthopedic Surgery San Diego provides high quality, expert orthopedic and musculoskeletal care, tailored to the specific needs of our patients. Orthopedic Surgery San Diego offers cutting-edge diagnostics, treatment, management and personalised care.
The expert multi-disciplinary team includes leading orthopaedic surgeons, pain management consultants, rheumatologists, allied specialists and radiologists. They work together to reduce pain, improve movement and make a real difference to patients’ lives.


