Knee Surgery, Knee pain treatment & Options in San Diego, CA
At Orthopedic Surgery San Diego, we offer superior minimally invasive options for every type of knee surgery, disease and symptom. Each knee surgery procedure we perform is supervised and administered by Dr. Robert Afra, whose longstanding experience at the forefront of orthopedic medicine has earned him a number of prestigious honors and patient recommendations. Dr. Afra provides cutting-edge surgical care including arthroscopic cartilage repair and ACL reconstruction, resurfacing techniques, partial knee replacement and total knee replacement. He places a premium on sound communication and lasting patient recovery, and works with you every step of the way to provide comprehensive, holistic treatment to restore your quality of life. If you’ve been told that you need knee surgery, we invite you to contact our knee surgery specialists to explore the various options at your disposal. We take pride in a patient-centered approach that addresses your questions and concerns throughout.
Our experience offers you practical ways to eliminate or reduce:
Knee injuries are some of the most debilitating events you can suffer. Whether you’ve torn the ligaments or broken a bone, the knee pain that accompanies such injuries can be paralyzing. Returning to everyday life and activities can be a challenge at best.
- Cartilage lesion
- Meniscus tear
- Patellofemoral syndrome
- Patellofemoral dislocation
- ACL tear
- PCL tear
- MCL tear
- Knee osteoarthritis
- Patellar tendinitis
- Quadriceps tendinitis
- Pes bursitis
- Shin splints
The knees are crucial joints that enable people to walk and perform other functions. Physical therapy often is effective in improving knee mobility and flexibility. In some cases, knee surgery is necessary to achieve long-term results. A range of surgical procedures can be employed to treat a variety of symptoms. Your experienced San Diego orthopedic surgeon will walk you through every step of the process, from imaging and diagnosis to knee surgery and postoperative care. Dr. Robert Afra is widely recognized as one of the nation’s leaders in the field of knee surgery. Dr. Afra was the Chief of Sports Medicine in the UCSD Department of Orthopedic Surgery, and today runs one of the most respected knee surgery clinics in San Diego. With access to cutting edge technologies and an experienced technical team, Dr. Afra is proud to offer the finest orthopedic surgical care in Southern California. We have helped thousands of patients from across the country achieve lasting relief from knee injuries and symptoms. If you would like to schedule your own knee surgery consultation today, please contact us to learn more about the available options.
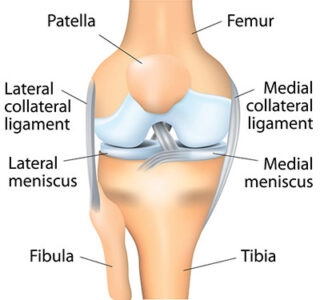
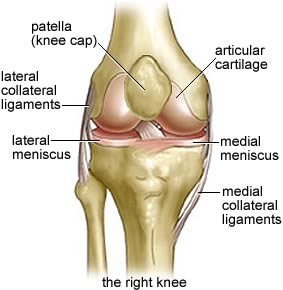
Knee Joint Description
ACL Tears
Because strenuous sports put a lot of stress on the knees, athletes often fall victim to ACL tears and sprains. About half of the time, patients with such conditions also suffer damage to other knee ligaments, the articular cartilage or the meniscus. Injured ligaments are considered “sprains” and are graded on a severity scale. A Grade 1 ACL sprain is the least severe, typically just an over-stretched ligament that does not impair normal knee function. A Grade 2 sprain involves a ligament stretched to the point that it is loose. This is sometimes called a “partial tear.” A complete tear, when the ligament is severed and the joint is unstable, is a Grade 3 sprain. According to the American Academy of Orthopaedic Surgeons, ACL injuries are caused by:
- Changing direction rapidly
- Stopping suddenly
- Slowing down while running
- Landing from a jump incorrectly
- Direct contact or collision, such as a football tackle.
Research indicates that women are particularly prone to ACL injuries. Certain sports, like football and basketball, are more of a threat to the knees than other physical activities. Symptoms include:
- A popping noise in the joint
- The knee giving out from under you
- Pain and swelling
- Loss of full range of motion
- Tenderness along the joint line
- Discomfort while walking.
A torn ACL does not heal on its own. Surgery is required to regain full function of the knee. Because the two sections of a severed ligament cannot be sutured back together, the ACL must be reconstructed by replacing it with a tissue graft on which a new ligament can grow. Graft material is taken from the patellar tendon, between the kneecap and the shin bone; the hamstring tendons, at the rear portion of the thigh; or the quadriceps tendon, which runs from the kneecap into the thigh. Surgeons sometimes graft tissue from cadavers. They perform the procedure by using an anthroscope to make small incisions. The operation involves less pain, shorter hospital stays and faster recovery times than more invasive surgery.
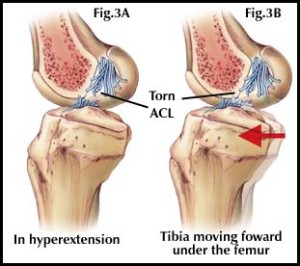
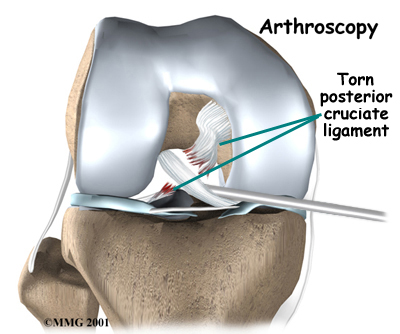
PCL Injuries
Because the posterior cruciate ligament is stronger than the ACL, it is more resilient to injury. The same three-stage severity scale used to evaluate ACL tears is employed to diagnose PCL injuries. It takes a powerful force to injure the PCL. Causes include: A direct blow to the front of the joint, like hitting the dashboard in a traffic accident or falling on a bent knee while playing sports; pulling or stretching the ligament, which can result in hyperextension; and stepping, walking or running in the wrong way. The symptoms of a PCL injury are:
- Pain in the back of the knee
- Swelling right after sustaining an injury
- Stiffness and difficulty walking
- A sense that the knee is about to give out.
In some cases, PCL injuries heal themselves and people regain full function of the knee. Physical therapy and nonsurgical procedures can be helpful. Knee Surgery is sometimes recommended, especially in the case of multiple injuries. For example, a patient might have a dislocated knee in addition to a PCL tear. As with the ACL, a torn PCL cannot be sewn back together. A tissue graft is required to rebuild it. Following knee surgery for an ACL or PCL injury, rehabilitation and recovery take six to 12 months. It is a challenging process, but the result is often a return to full function of the knee.
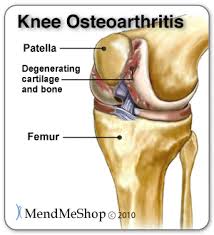
Knee Osteoarthritis
If your knee becomes inflamed due to arthritis, you will experience pain, swelling and stiffness. Left untreated, the discomfort and loss of mobility can progress and cause disability. While arthritis may occur in any joint, it is most often diagnosed in knees. There is no cure for arthritis, but treatment and knee surgery can relieve the symptoms and restore function. A layer of articular cartilage covers the three bones that connect in the knee, preventing them from rubbing against one another when the joint is flexed. Two other pieces of cartilage, called meniscus, form a cushion between the thighbone and shinbone. The synovial membrane, a lining around the joint, emits a lubricant into the cartilage. Osteoarthritis results from the gradual deterioration of the cartilage. Without this cushioning substance, inflammation and bone spurs can develop. This is the most commonly diagnosed type of knee arthritis. The condition worsens until it becomes difficult to bend or straighten the knee. The joint might buckle, lock in one position, make clicking or grinding noises, and get worse when the humidity rises. Other symptoms are redness, warmth and tenderness; and decreased range of motion. Medication, physical therapy and other methods can relieve some of the suffering. Another treatment, viscosupplementation, involves the injection of stem cells or platelet-rich plasma from your own body into the joint. Sometimes, knee surgery is necessary. Among the common procedures are:
- Arthroscopy, in which a surgeon makes a small incision and uses a thin instrument to diagnose and treat degenerated tissues;
- Cartilage grafting, the transplanting of healthy cartilage from another part of the knee or from a tissue bank;
- Osteotomy, in which a surgeon cuts and reshapes the shinbone or thighbone to take pressure off the joint; and
- Anthroplasty, the total or partial replacement of the knee with metal or plastic materials.
Knee Osteoarthritis Treatment Options
Analgesics/NSAIDS Use
Injections
Topical Lotions
Dietary Supplements
Physical Interventions
Exercise
Unloader Braces
Medial
Lateral
Patellar-Femoral
Procedures:
Opening Wedge Osteotomy of the Tibia (High Tibial Osteotomy)
Opening Wedge, Distal Femoral Osteotomy
Unicompartmental Knee Arthoplasty, Medial Mobile or Fixed Bearing
Total Knee Replacement
Arthroscopy for Osteoarthritis
Patellar Tendonitis
Quadriceps Tendonitis
Pes Bursitis
Inflammation of the bursa, between the shinbone and the hamstring muscle tendons, is called pes anserine bursitis. Bursae are small sacs containing a fluid that cushions joints. Inflammation results when the bursa produces excess fluid and causes swelling. The main symptoms are pain and tenderness on the inside of the knee, two or three inches below the join. The condition occurs due to overuse, or repetitive friction irritating the bursa. Runners and other athletes are especially vulnerable. Among the causes of pes bursitis are:
- Improper training methods, like failing to stretch
- Excessive running on hills, or a sudden increase in running distance;
- Tight hamstring muscles
- Obesity
- Turning out the knee or lower leg;
- Osteoarthritis in the knee
- A medial meniscus tear.
The first remedies to try are rest, ice treatments, anti-inflammatory medication and physical therapy. In advanced cases, knee surgery involving surgical removal of the bursa is necessary. The procedure frequently is performed on an outpatient basis.
Shin Splints
The common term for pain along the inner edge of the shinbone is shin splints. The condition usually develops following exercise, with runners and dancers among those most at risk. Technically known as medial tibial stress syndrome, shin splints are characterized by inflammation of the muscles, tendons and bone tissue around the shinbone. The pain occurs where the muscles connect to the bone. Causes of shin splints include:
- Strenuous physical activity
- Sudden changes in workout routines
- Flat feet or rigid arches
- Exercising with inadequate shoes.
Rest, ice, medication, stretching exercises, orthotics and elastic compression bandages often relieve the symptoms. Knee Surgery to remove the fascia (tissue around the muscles) could be needed if a patient’s condition involves compartment syndrome, or if the pain is extreme. When a muscle has been torn away from the shinbone, knee surgery is necessary to reattach the muscle.









