Shoulder Replacement
Shoulder Replacement Surgery
We offer a holistic approach to shoulder replacement surgery at San Diego Orthopedic Surgery, rather than simply focusing on a single point source of patient distress, our advanced imaging and diagnostic tools analyze the full joint for anything amiss. Dr. Robert Afra is widely renowned as one of the foremost shoulder replacement surgery expert and orthopedic surgeons in the nation, his experience leads an expert team of technicians and medical professionals in every shoulder replacement surgery procedure we offer. Our focus is on the total patient, so we consistently exhaust all nonsurgical options before considering a more permanent approach such as shoulder replacement surgery. This includes a variety of minimally invasive options such as therapy and non-operative treatment.
If shoulder replacement surgery is necessary, we offer a diverse selection of procedures to relieve all major issues
Shoulder replacement surgery, also known as shoulder arthroplasty, is a surgical procedure in which a damaged or diseased shoulder joint is replaced with an artificial joint or prosthesis. This procedure is typically performed to relieve pain, improve mobility, and restore function in the shoulder when other non-surgical treatments have not been effective.
The shoulder joint is a ball-and-socket joint, where the head of the upper arm bone (humerus) fits into a shallow socket in the shoulder blade (scapula). Conditions such as osteoarthritis, rheumatoid arthritis, traumatic injuries, and other degenerative joint diseases can lead to the deterioration of the shoulder joint, causing pain and limited range of motion.
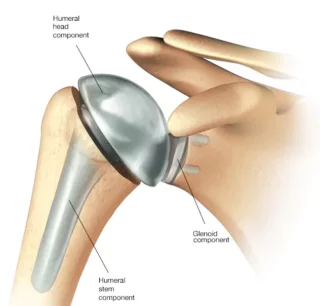
During shoulder replacement surgery, the damaged parts of the shoulder joint are removed, and the artificial components are implanted. The artificial joint typically consists of a metal ball attached to a stem that is inserted into the upper arm bone and a plastic socket that is implanted into the shoulder blade. In some cases, the surgeon may replace only the ball or only the socket, depending on the extent of the damage.
When You Need Shoulder Replacement Surgery?
The shoulder functions as a ball-and-socket joint, characterized by a large ball and a shallow socket, allowing for a greater range of motion than any other joint in the body. This configuration is analogous to a golf ball and tee. The shoulder’s stability hinges on the surrounding soft tissues, including the muscles and tendons forming the rotator cuff, as well as the shoulder capsule, a ligament encircling the joint.
Articular cartilage covers the joint surfaces, facilitating smooth, frictionless movements. The rotator cuff muscles play a crucial role in maintaining the central positioning of the shoulder. Arthritis can manifest in two ways within the shoulder joint: osteoarthritis, affecting the joint with an intact rotator cuff, and rotator cuff arthropathy, occurring when degenerative rotator cuff tears lead to irreparable damage. In the latter case, the humeral head becomes decompensated, causing superior migration and resulting in impingement, pain, and stiffness, akin to pseudo paralysis.
The choice of joint replacement depends on the type of arthritis present. An arthritic shoulder with an intact rotator cuff necessitates a total shoulder replacement that replicates the natural shoulder joint anatomy. Rotator cuff arthropathy calls for a reverse shoulder replacement, wherein the ball and socket are switched to enhance shoulder function, relying on the outer deltoid muscle for power. This type of replacement is also utilized in treating certain shoulder fractures, especially in the elderly population, to enhance functionality.
Additionally, trauma contributes to the development of shoulder arthritis. If the upper arm bone’s head is shattered, attempting to fix the fracture may yield a poor outcome with persistent pain and impaired function, prompting the recommendation for shoulder replacement. This scenario is particularly prevalent in older patients with osteoporosis.
Types Of Shoulder Replacement Surgery
There are a range of surgical options for shoulder replacement, depending on whether you have an intact rotator cuff or not. After careful examination and reviewing your MRI and CT scans, your consultant will make a decision about which implant would be appropriate for you.
Typically, if your rotator cuff is intact, you will get an anatomic or total shoulder replacement. If the rotator cuff is torn, your consultant will perform a reverse shoulder replacement.
There are different types of humeral implants which are long stem, short stem and stemless. These all depend on your bony anatomy and your consultant will discuss these options with you and plan your operation depending on these criteria. The implants are most commonly made of metal including titanium, cobalt chrome alloys, polyethylene. Ceramic shoulder replacements can be used; however, these are relatively new and there are currently no studies comparing the outcomes with other materials.
The new generation of short stems or stem less implants provide better restoration of normal anatomy in young patients where bone preservation is vital. These need a less invasive technique to insert and work to conserve bone stock, allowing for easy revision in the future if this is required.
Options for shoulder replacement surgery include:
Stemmed hemiarthroplasty: only the ball at the top of the humerus is replaced using a metal stem that sits inside the upper arm bone with a metal ball on the top. This type of surgery may be used if the humerus is severely fractured, but the socket remains in good condition.
Resurfacing hemiarthroplasty: This entails replacing just the joint surface at the head of the humerus with a cap-like prosthesis but no stem. This type of surgery may be recommended if you have intact cartilage in the shoulder socket (glenoid) or if there is no fracture of the humeral neck or head. It is ideal for younger or very active patients as it does not carry the same risk of components wearing and loosening that comes with total shoulder replacement.
Total shoulder replacement Surgery: the arthritic joint is completely replaced with an artificial implant consisting of a polished metal ball and a plastic socket. If your bone is in good condition the surgeon may use a press-fit component. However, if the bone is soft, bone cement may be used to hold the components in place.
Reverse shoulder replacement Surgery: Conventional shoulder replacement surgery is not suitable for patients with large tears in the rotator cuff who have developed a form of shoulder arthritis called cuff tear arthropathy. For these patients, reverse shoulder replacement is the only definitive surgical treatment. Whereas conventional shoulder replacement mimics the normal anatomy of the shoulder, with a plastic cup fitting into the shoulder socket and a metal ball at the top of the upper arm, in reverse shoulder replacement the metal ball is fitted into the socket and the plastic cup is attached to the upper end of the humerus. Rather than relying on the rotator cuff muscles to move the arm, a reverse total shoulder replacement uses the deltoid muscles. The result is a dramatic reduction in pain from arthritis with a better range of movement for people with cuff tear arthropathy.
Balloon shoulder arthroplasty is another ground-breaking surgical procedure to treat the pain associated with major irreparable rotator cuff tears. It entails inserting a balloon-shaped device above the shoulder joint to create a physical barrier between the bones to reduce pain, improve shoulder function and delay more invasive surgery. The spacer dissolves naturally after around a year.
Shoulder Arthritis: An Evidence-Based Overview
Introduction
Shoulder arthritis is a degenerative condition characterized by the deterioration of the cartilage and tissues surrounding the shoulder joint, leading to pain, stiffness, and reduced range of motion. This overview aims to summarize the findings of prospective randomized controlled studies in the management and treatment of shoulder arthritis.
Etiology
There are multiple types of shoulder arthritis, including osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis. Each type has distinct underlying mechanisms but commonly leads to joint degeneration over time.
Clinical Presentation
Patients usually complain of persistent shoulder pain that worsens with activity, limited range of motion, and stiffness. Some may also experience crepitus, a cracking sound, during shoulder movements.
Diagnosis
Diagnostic techniques usually involve imaging studies like X-rays and MRI, along with physical examinations and patient history. Newer diagnostic modalities are under investigation for their effectiveness.
Treatment Options
Conservative Management
Initial treatment often involves a combination of physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections. Some studies indicate that early conservative treatment can slow down the progression of the disease.
Surgical Options
Shoulder arthroplasty and joint replacement are often recommended for severe cases. Several studies have demonstrated the effectiveness of these surgical interventions in improving function and reducing pain.
Future Directions
New therapies, including gene therapy and tissue engineering, are currently under investigation. Preliminary studies suggest promising outcomes but are yet to be validated in larger, randomized controlled trials.
Conclusion
Shoulder arthritis is a debilitating condition that significantly impacts the quality of life. The current treatment landscape involves conservative and surgical options, each with its own set of pros and cons. Further research is needed to establish the effectiveness of emerging therapies.
Massive Rotator Cuff Tears: An Evidence-Based Overview
Introduction
Massive rotator cuff tears represent a severe form of shoulder injury that involves tearing of two or more of the rotator cuff tendons. They result in significant pain and functional impairment. This review aims to summarize the findings from prospective randomized controlled trials on the diagnosis and management of massive rotator cuff tears.
Pathophysiology
Massive rotator cuff tears often result from acute trauma or degenerative changes. In either case, the functional anatomy of the shoulder joint is compromised, leading to instability, pain, and reduced range of motion.
Clinical Presentation
Patients usually present with severe shoulder pain, limited range of motion, and muscle weakness. In some cases, the tear may be asymptomatic initially but become painful over time.
Diagnostic Approaches
The diagnosis typically involves a combination of clinical evaluation and imaging studies, such as MRI and ultrasound. MRI remains the gold standard for assessing the size and extent of the tear.
Treatment Modalities
Conservative Treatment
Physical therapy and corticosteroid injections are among the conservative treatment options. However, conservative management has limited effectiveness in treating massive tears according to some studies.
Surgical Options
Surgical options include rotator cuff repair, tendon transfer, and reverse total shoulder arthroplasty. Randomized controlled studies suggest that surgical interventions are more effective than conservative treatment in improving function and reducing pain for massive tears.
Rotator Cuff Repair
Open or arthroscopic repair of the torn tendons is a common surgical option. Some studies have shown good outcomes in terms of pain relief and functional improvement.
Tendon Transfer
For irreparable tears, tendon transfers have been shown to be effective in restoring some level of function.
Reverse Total Shoulder Arthroplasty
In older patients or those with concomitant arthritis, reverse total shoulder arthroplasty has demonstrated good outcomes in terms of both pain and function.
Future Directions
Emerging treatments like biologics and tissue engineering are under investigation. These therapies aim to facilitate tendon healing and are currently in the experimental stage9.
Conclusion
Massive rotator cuff tears are a complex and disabling condition that require multidisciplinary intervention. Current evidence suggests that surgical treatment is generally more effective than conservative management for this particular subset of rotator cuff injuries.
Anatomic Total Shoulder Arthroplasty: An Evidence-Based Overview
Introduction
Anatomic total shoulder arthroplasty (aTSA) is a surgical procedure designed to alleviate pain and improve function in patients with shoulder joint degeneration, primarily due to osteoarthritis or rotator cuff arthropathy. This review aims to summarize findings from prospective randomized controlled trials concerning the effectiveness and challenges of aTSA.
Indications
Anatomic total shoulder arthroplasty is generally indicated for patients with severe osteoarthritis, rotator cuff arthropathy, or post-traumatic arthritis who have failed conservative treatment.
Surgical Technique
The surgery involves replacing the degenerated humeral head and glenoid with prosthetic components. The surgical approach and the type of implant can vary, but recent studies have focused on optimizing component positioning to improve postoperative outcomes.
Postoperative Outcomes
Pain Relief
Randomized controlled studies have demonstrated significant pain relief following aTSA, with many patients reporting substantial improvement as early as 6 weeks postoperatively.
Functional Improvement
Functional outcomes, measured using validated scoring systems like the Constant-Murley score or the American Shoulder and Elbow Surgeons (ASES) score, have also shown marked improvement following surgery.
Complications
While aTSA has a generally low complication rate, issues such as implant loosening, infection, and nerve injury have been reported. Proper surgical technique and postoperative care are crucial for minimizing these risks.
Comparative Studies
Some studies have compared aTSA with other surgical options like hemiarthroplasty and reverse total shoulder arthroplasty. Generally, aTSA has been found to provide better functional outcomes for patients with an intact rotator cuff.
Rehabilitation
Rehabilitation is essential for optimal postoperative outcomes. A structured physical therapy program, usually initiated a few weeks after surgery, has been shown to be effective in restoring function.
Conclusion
Anatomic total shoulder arthroplasty is an effective surgical option for patients with end-stage shoulder degeneration who have not responded to conservative treatments. While the procedure is generally safe and effective, appropriate patient selection, surgical technique, and postoperative care are critical for success.
Reverse Total Shoulder Arthroplasty: An Evidence-Based Overview
Introduction
Reverse Total Shoulder Arthroplasty (rTSA) is a surgical procedure increasingly used for a variety of shoulder pathologies, particularly in cases where the rotator cuff is compromised. This overview aims to summarize findings from prospective randomized controlled trials concerning its efficacy, complications, and long-term outcomes.
Indications
rTSA is commonly indicated for patients with rotator cuff tear arthropathy, severe shoulder fractures, or complex proximal humerus fractures, especially in elderly patients.
Surgical Technique
In rTSA, the ball and socket components of the shoulder joint are reversed to improve mechanical advantage and allow the deltoid muscle to take over the function of the rotator cuff.
Efficacy
Pain Management
Multiple studies have demonstrated that rTSA is effective in providing significant pain relief in the majority of patients.
Functional Outcomes
Functional outcomes tend to be better in patients with lower preoperative functional scores. Randomized trials have reported improvements in shoulder movement and strength following rTSA.
Complications
Potential complications include scapular notching, infection, and instability. Studies show that complication rates can be minimized with meticulous surgical technique and appropriate patient selection.
Comparison with Anatomic Total Shoulder Arthroplasty (aTSA)
While aTSA remains the treatment of choice for patients with intact rotator cuffs, rTSA has been found to provide better outcomes in those with significant rotator cuff pathology.
Rehabilitation
Postoperative rehabilitation plays a significant role in achieving optimal outcomes. Controlled, phased rehabilitation has been shown to be beneficial in multiple prospective studies.
Long-Term Outcomes
Data from long-term studies indicate good implant survivorship and sustained functional benefits over time, although some decline can be expected due to the natural aging process.
Conclusion
Reverse Total Shoulder Arthroplasty is a valuable tool in the treatment of complex shoulder pathologies, particularly in older patients or those with compromised rotator cuffs. While generally effective in improving function and relieving pain, careful patient selection and postoperative management are key to minimizing complications and maximizing long-term benefits.
Role of Reverse Total Shoulder Arthroplasty in Massive Rotator Cuff Tears: An Evidence-Based Overview
Introduction
Massive rotator cuff tears pose significant challenges in treatment, often leading to shoulder dysfunction and pain. Reverse total shoulder arthroplasty (rTSA) has emerged as an effective surgical solution. This review aims to summarize findings from prospective randomized controlled trials regarding the role of rTSA in treating massive rotator cuff tears.
Indications for rTSA in Massive Rotator Cuff Tears
rTSA is indicated in cases of massive rotator cuff tears accompanied by severe pain, dysfunction, or associated cuff tear arthropathy that is unresponsive to conservative treatment.
Efficacy
Pain Relief
Studies have demonstrated that rTSA provides significant pain relief and improves quality of life for patients with massive rotator cuff tears.
Functional Outcomes
Randomized controlled trials show that rTSA can improve shoulder motion and strength, especially in patients with preoperative limitations.
Comparative Analysis: rTSA vs Other Surgical Options
rTSA has shown better postoperative functional scores compared to other surgical options like tendon transfer or partial cuff repair in patients with massive rotator cuff tears.
Complications Specific to Massive Rotator Cuff Tears
The risks of scapular notching and instability may be higher in these patients. Proper surgical technique is crucial to minimize such risks.
Rehabilitation
Postoperative rehabilitation strategies, often involving range-of-motion and strengthening exercises, are vital. Controlled, phased rehabilitation programs have shown effectiveness in randomized trials.
Long-term Outcomes
Long-term studies indicate that benefits such as pain relief and functional improvements are sustained over time, although a decline due to natural aging is to be expected.
Conclusion
Reverse total shoulder arthroplasty plays a pivotal role in the management of massive rotator cuff tears, particularly when conservative treatments have failed. Randomized controlled trials consistently support its efficacy in improving both pain and functional outcomes, although careful patient selection and postoperative management are key to optimal results.
Role of Reverse Total Shoulder Arthroplasty in Proximal Humeral Fractures: An Evidence-Based Overview
Introduction
Proximal humeral fractures are common, especially among the elderly. When conservative treatments fail or are inappropriate, surgical options, including reverse total shoulder arthroplasty (rTSA), are considered. This review aims to present an evidence-based discussion based on prospective randomized controlled studies.
Indications
rTSA is particularly indicated in elderly patients with complex, comminuted proximal humeral fractures or in those who have both a fracture and significant rotator cuff pathology.
Efficacy
Pain Relief
rTSA has been demonstrated to offer immediate and substantial pain relief, making it a desirable option for this patient population.
Functional Outcomes
Randomized studies indicate that patients experience improved range of motion and daily function following rTSA for proximal humeral fractures.
Surgical Technique
The success of rTSA relies on various factors including the choice of implant, proper alignment, and meticulous surgical technique to minimize complications like scapular notching.
Comparison to Other Surgical Techniques
Several studies comparing rTSA to hemiarthroplasty or open reduction and internal fixation (ORIF) found superior functional outcomes and patient satisfaction with rTSA.
Complications
Common complications include infection, dislocation, and implant failure. However, complication rates are generally low when the procedure is performed by experienced surgeons.
Rehabilitation
Effective rehabilitation protocols generally consist of early passive motion followed by gradual active exercises. Randomized studies endorse structured, personalized rehabilitation plans.
Long-Term Outcomes
Though long-term studies are limited, existing evidence suggests that the functional and pain relief benefits of rTSA are durable, albeit with some age-related decline.
Conclusion
Reverse total shoulder arthroplasty serves as a viable and effective treatment option for complex proximal humeral fractures, particularly in elderly patients or those with concurrent rotator cuff pathology. Its efficacy in providing pain relief and improving function is supported by numerous prospective randomized controlled studies.
Role of Reverse Total Shoulder Arthroplasty Over Anatomic Shoulder Arthroplasty in the Elderly: An Evidence-Based Overview
Introduction
Both reverse total shoulder arthroplasty (rTSA) and anatomic shoulder arthroplasty (aTSA) are surgical options for shoulder joint pathology. The choice between these two techniques is a subject of ongoing study, particularly in the elderly population. This review summarizes findings from prospective randomized controlled studies to determine which approach may be preferable in elderly patients.
Clinical Indications
Both procedures are indicated for end-stage osteoarthritis, but rTSA is often recommended for patients with compromised rotator cuffs, a common condition among the elderly.
Efficacy
Pain Management
Studies indicate that both rTSA and aTSA provide significant pain relief. However, rTSA seems to have a slight advantage in cases where the rotator cuff is compromised.
Functional Outcomes
Functional recovery in terms of range of motion and activities of daily living is generally better in rTSA when compared to aTSA in the elderly population, especially those with rotator cuff deficiencies.
Surgical Technique and Implant Considerations
aTSA requires an intact rotator cuff for optimal outcomes, whereas rTSA can be successful even when the rotator cuff is compromised. The latter is often the case in elderly patients.
Complications
Both procedures carry the risk of complications such as infection, dislocation, and implant failure. However, complication rates in rTSA have been found to be slightly higher.
Rehabilitation
Effective postoperative rehabilitation is essential for both procedures. However, studies suggest that patients undergoing rTSA may require a less stringent rehabilitation program.
Cost-effectiveness
Although rTSA is generally more expensive, its potentially better outcomes in terms of function and pain relief in the elderly population may justify the higher initial costs.
Long-term Outcomes
Data indicates that rTSA may offer superior long-term outcomes in the elderly, particularly in terms of sustained pain relief and functional improvement.
Conclusion
For the elderly population, especially those with compromised rotator cuffs, evidence from prospective randomized controlled studies suggests that rTSA may be preferable to aTSA in terms of both functional outcomes and pain management, despite slightly higher complication rates and costs.









