Knee Osteoarthritis
Introduction
Symptoms of Knee Osteoarthritis
Pain
Knee pain is the primary clinical complaint of individuals with OA. Initially, pain may only occur with activity. As Knee Osteoarthritis advances, pain becomes more constant and disruptive. Typical descriptions include an achy, throbbing pain that is worse with weight bearing. Night pain and rest pain often develop in late-stage OA. Swelling, joint stiffness, and crepitus commonly accompany Knee Osteoarthritis knee pain. The severity often fluctuates, with weather changes and overactivity aggravating symptoms.
Functional Impairments
Progressive loss of knee function parallels increasing pain in Knee Osteoarthritis. Activities like walking, rising from a chair, and stair climbing become progressively more difficult. Eventual limitations in daily tasks reduce independence and quality of life. Quadriceps weakness and altered gait mechanics contribute to functional decline. Patient-reported outcome scores quantify Knee Osteoarthritis impact on physical function. Scores worsen an average of 3-4% yearly as Knee Osteoarthritis advances.
Instability and Buckling
The degenerative process diminishes knee stability in some Knee Osteoarthritis patients. Laxity coupled with muscle weakness leads to episodes of buckling, shifting, or giving way. This causes concern about falling and avoidance of activities. Varus or valgus thrust seen on examination may indicate worsening instability. However, joint laxity does not correlate with radiographic disease severity or pain levels.
Range of Motion Loss
Joint stiffness and reduced range of motion frequently accompany Knee Osteoarthritis. Contracture first develops in knee extension, followed by flexion loss in late-stage disease. Heberden’s nodes visible at the finger joints reflect an underlying generalized limitation in mobility. Morning gelling and difficulty initiating movement are common complaints. Range of motion declines approximate 1-3 degrees yearly as Knee Osteoarthritis progresses. In summary, the cardinal symptomatic features of knee OA include chronic pain, progressive functional impairment, episodic instability, and worsening stiffness or mobility loss. These symptoms often severely reduce quality of life and ability to remain active. Understanding the typical clinical presentation is key for appropriate management.
Radiographic Findings of Knee Osteoarthritis
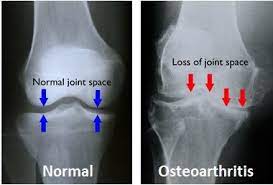
Radiography is the primary imaging modality for diagnosing and staging knee osteoarthritis (OA). Characteristic radiographic features allow assessment of Knee Osteoarthritis severity and progression over time. Understanding the typical radiographic presentation of knee OA is important for clinical decision making and monitoring.
Features of Early Osteoarthritis
The earliest radiographic sign of knee Knee Osteoarthritis is joint space narrowing, indicating loss of cartilage. This begins medially, reflecting higher loads transmitted across this compartment. Additional early findings include subchondral sclerosis, osteophyte formation, and subcortical cysts at the tibia and femur. Synovial thickening and suprapatellar joint effusions may also be present. These changes often first manifest 2-4 years after knee injury.
Progression of Joint Space Narrowing
Gradual progression of medial joint space narrowing is the hallmark finding of advancing knee Knee Osteoarthritis. Laterally, the joint space remains preserved until end-stage disease. Each 1 mm of joint space loss increases medial compartment loads by up to 20%. Loss of 50% medial joint space height predicts poor clinical outcomes. Quantifying and tracking joint space width allows assessment of Knee Osteoarthritis severity and progression.
Additional Structural Changes
As OA progresses, marginal osteophytes enlarge and subarticular cysts become more pronounced. Accessory ossicles may develop in tendon attachments. Full thickness loss of articular cartilage leads to bone-on-bone apposition and subchondral sclerosis. Eventually the lateral compartment also narrows significantly, indicating end-stage changes. Knee malalignment accelerates joint deterioration, especially with varus or valgus thrust.
Correlation to Symptoms and Function
The severity of radiographic knee Knee Osteoarthritis only moderately correlates to symptoms like pain and stiffness. Up to 50% of those with radiographic changes are asymptomatic. However, advanced imaging confirms structural deterioration does relate to functional decline. Radiographs best identify macroscopic Knee Osteoarthritis progression rather than symptomatic changes.
In summary, serial radiographs looking for joint space narrowing provide the standard diagnostic imaging for knee OA. Correlation with advanced imaging and clinical findings allows optimal assessment of disease status.
Nonoperative Management of Knee Osteoarthritis
Nonoperative management focused on symptom relief and maintenance of function is the cornerstone of knee osteoarthritis (OA) treatment. Common strategies include weight loss, physical therapy, medications, injections, bracing, and activity modification. Evidence supports various nonsurgical approaches for initial Knee Osteoarthritis management.
Patient Education
Educating patients about OA pathophysiology, treatment options, and self-management helps empower involvement in care. Patient education correlates with increased adherence to recommended treatments and exercise. Information on activity modification, joint protection during tasks, and weight management is essential.
Exercise Therapy
Supervised exercise provides short and long-term symptomatic relief while improving function in knee OA. Aquatic exercises, individualized strength training, and neuromuscular re-education are most beneficial. Tai chi and yoga help improve balance and proprioception. Adherence is crucial for sustained improvements.
Weight Loss
Reducing body mass lessens joint loads and inflammation, correlating with OA pain relief.5 Each 1 kg of weight loss reduces knee joint loads by 4 kg. A 5-10% loss of body weight reduces OA symptoms 20-50%. Dietary changes and increased activity facilitate weight reduction.
Bracing and Assistive Devices
Unloader braces and lateral heel wedges aim to reduce medial compartment pressures. Canes and walkers relieve weightbearing stresses. Evidence for sustained bracing benefits is limited, but periodic use may help during flares.
Medications
Topical NSAIDs provide local analgesia with minimal systemic effects. Oral NSAIDs and acetaminophen are used short-term for flares. Tramadol or opioids can be considered for refractory pain if risks are acceptable. Hyaluronic acid injections may provide up to 6 months symptom relief.
Activity Modification
Avoiding high-impact activities helps prevent OA exacerbations. Pacing and scheduling rest periods makes tasks more tolerable. Assistive devices facilitate weightbearing activities like standing or walking. Activity modification aims to maintain current function rather than worsening symptoms.
In summary, a combination of nonsurgical treatments offers the best results for knee OA. Patient participation in the management plan is key. Surgery is reserved for severe, refractory cases or joint failure.
HA Viscosupplementation vs PRP for Knee Osteoarthritis
Intraarticular injections provide symptomatic relief for knee osteoarthritis (OA) patients who have failed conservative treatment. The two leading options are hyaluronic acid (HA) viscosupplementation and platelet-rich plasma (PRP). Multiple randomized trials allow comparison of their clinical efficacy.
Mechanisms of Action
Exogenous HA aims to restore the viscoelastic properties of synovial fluid, which are reduced in Knee Osteoarthritis. HA may also have anti-inflammatory effects. In contrast, growth factors concentrated in PRP act on joint tissues to potentially stimulate cartilage repair and inhibit inflammatory mediators. The biologic mechanisms differ, but both aim to improve joint homeostasis.
Onset and Duration of Relief
Patients report significant pain relief as early as 2 weeks after PRP injection, with peak effects at 8 weeks. HA injections elicit more gradual onset of symptom relief, taking 4-6 weeks to maximize benefits. However, HA effects last significantly longer. Pain reduction persists up to 26 weeks after HA injection, while PRP benefits subside after 6-9 months. Repeat injections can prolong durability of both treatments.
Functional Outcomes
Both HA and PRP injections improve self-reported function in knee Knee Osteoarthritis patients based on validated outcome scores. HA provides sustained functional benefits up to 26 weeks.6 PRP also significantly improves short-term function, but gains attenuate after 6 months. The treatments are comparable regarding functional improvement in the first 3-6 months.
Radiographic Disease Progression
There is no evidence that either HA or PRP injections slow structural progression of knee OA based on joint space narrowing. Both provide purely symptomatic relief without disease-modifying effects. However, symptom control facilitates retention of functional abilities, which is the primary goal.
Frequency of Repeat Injections
The longer duration of HA effect allows less frequent repeat injections, with typical spacing of 6 months. PRP requires more frequent repeating, often at intervals of 3-4 months, due to faster waning of benefits. Over 2-3 years, patients receive 30-50% fewer HA injections compared to PRP. This makes HA potentially more cost-effective long-term. In summary, both HA and PRP offer comparable symptomatic relief in knee OA. PRP works faster, but HA provides more sustained benefit. The choice involves balancing onset versus duration when determining injection frequency. Further study on optimizing PRP preparations may prolong its effects.
Bracing for Symptomatic Knee Osteoarthritis
Bracing is a potential treatment option aimed at unloading damaged knee joint compartments in Knee Osteoarthritis (OA). Evidence supports bracing for short-term symptomatic relief, but effects on long-term outcomes remain unclear. Appropriate patient selection is important.
Proposed Mechanisms
Braces and orthotics mechanically unload the affected compartment by applying a corrective force. This aims to redistribute forces away from arthritic areas vulnerable to compressive loads. Additionally, many braces provide added stability and proprioceptive feedback that could reduce pain with movement.
Types of Braces
Knee braces fall into main categories: prophylactic/rehabilitative, functional, and unloader braces. For Knee Osteoarthritis, unloader braces are most appropriate to provide compartment offloading. These rigid braces have condylar pads that apply a corrective force, usually medially for medial compartment Knee Osteoarthritis.
Effect on Pain and Function
In the short-term, unloader bracing over 6 weeks-6 months consistently demonstrates pain reduction in knee OA versus no bracing. Improvements in function scores, walking speed, and balance are also seen. However, patient compliance with brace use tends to decline over time. Extended use over 1-2 years shows more variable functional benefits.
Effect on Knee Adduction Moment
The knee adduction moment reflecting medial compartment load is lowered by 5-10% with bracing based on gait studies. However, this does not strongly correlate to symptom changes, perhaps due to brace migration. The durability of biomechanical effects, like the clinical effects, remains questionable.
Candidates for Bracing
Ideal candidates for unloader bracing have symptomatic, unicompartmental Knee Osteoarthritis with biomechanical alignment amenable to offloading. Varus or valgus OA patterns respond best. Bracing should be avoided in severe tricompartmental OA or with significant rotational deformities.
Potential Adverse Effects
Documented risks of knee bracing include skin irritation, added stresses to other joints, and muscle atrophy if overused. These issues can limit tolerance. Braces are also costly and often not covered by insurance plans. Careful patient selection and treatment goals are warranted. In summary, compartment unloader braces can provide symptomatic relief for knee OA short-term, but long-term superiority over other conservative measures is unproven. Appropriate patient selection, education, and monitoring are necessary to maximize benefits while minimizing potential downsides of bracing.
Indications for Unicompartmental vs Total Knee Arthroplasty
End-stage knee osteoarthritis refractory to conservative treatment may warrant surgical management with arthroplasty. The primary options include unicompartmental knee arthroplasty (UKA) or total knee arthroplasty (TKA). Selection criteria differ based on disease distribution and patient factors.
Unicompartmental Osteoarthritis
Isolated medial or lateral compartment osteoarthritis with full thickness cartilage loss is the classic indication for UKA. Preserved cartilage in other compartments is required. Up to 20% joint space narrowing may be acceptable in other areas. Varus or valgus deformity should be correctable to neutral alignment. UKA is not appropriate for patellofemoral disease.
Age
Younger patients are better candidates for UKA given higher activity demands. Older, sedentary patients place lower stresses across the arthroplasty so TKA longevity is less crucial. UKA aims to more closely restore native knee kinematics for high function. The 10-year survival averages 95% for UKA patients under age 65.
Demand Level
UKA facilitates high flexion activities and normal gait mechanics compared to TKA. Thus, UKA is preferred for manual laborers or athletes desiring higher function. However, TKA reliability may outweigh kinematic advantages of UKA in lower demand elderly patients.
BMI
Lower body mass index (BMI) below 35 is preferred for UKA success, as higher BMIs increase wear and aseptic loosening risks.5 The minimally invasive approach also becomes more difficult with higher BMI. For obese patients, TKA is generally more appropriate.
Contralateral Knee Status
A contralateral healthy knee or UKA allows better comparison and rehabilitation after UKA. Patients with prior contralateral TKA do worse with UKA on the opposite side and should match with TKA instead.7 Limb asymmetry after different procedures should be avoided. In summary, UKA offers advantages for younger, active patients with isolated unicompartmental osteoarthritis and lower BMI. TKA remains preferable for older, less active patients with multipartite disease, high BMI, or prior knee replacements. Thorough assessment provides optimal implant selection.


